For Your Heart's Sake - Dial 911
February 28, 2021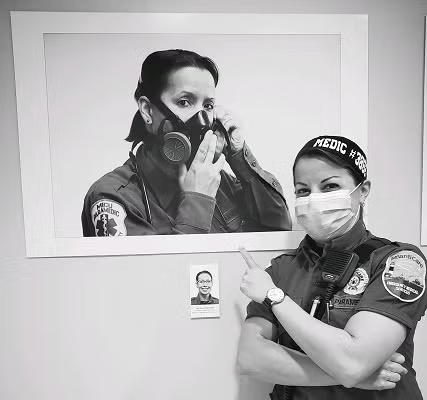
By Jade Russell, MICP, and Trish Russell, MICP, NREMT-P
AtlantiCare Regional Medical Center Emergency Medical Services
There’s characteristically an apologetic comment we hear when we respond to a call for symptoms of a heart attack.
“I’m sorry I called you out in the middle of the night. I didn’t want to disturb you.”
“I thought I’d feel better if I just rested.”
“I thought I just had indigestion.”
Time does matter when it comes to a heart attack.
What does bother us is when people put off seeking care for symptoms of a heart attack. It is heartbreaking to us when we know we could have saved a life if an individual or loved one had dialed 911.
During a heart attack, the heart muscle doesn’t get enough blood flow – which can damage the heart and lead to death.
People putting off dialing 911 for heart attack symptoms is not new.
As paramedics, we have a unique perspective on this. One of us (Jade), works nights and the other (Trish) works days.
Elderly individuals sometimes call their adult children about their symptoms, rather than dialing 911 themselves. Their children make the call for them.
In other cases, individuals seem to know something is wrong but they put off calling for help because they’re afraid of the diagnosis. To them, they can’t possibly be having a heart attack unless a medical professional evaluates them. If they don’t get evaluated, they won’t get that confirmed diagnosis. Denial won’t make the problem go away and it could prevent the person from getting critical life-saving treatment. We sometimes see this among couples. The individual experiencing symptoms does not want to “abandon” his or her loved one. This is especially true if the individual is the primary caregiver for the family member.
In other situations, symptoms are so subtle that people dismiss them.
Of course, over the last year, we’ve also experienced the national pandemic-spurred trend of people putting off dialing 911 for symptoms of heart attack and other life-threatening illnesses. They’re afraid of catching COVID-19 or they don’t want to be separated from their loved ones.
We and our EMS colleagues recognize the above fears and concerns and others that people have.
We’ve taken extraordinary measures to care for patients safely throughout the pandemic. Like hospitals throughout New Jersey, we’ve adjusted our visitor policy throughout the pandemic based on state and federal guidelines. We’ve done so as we’ve focused on safety and in consideration of the important role family members and others play when a loved one is hurt or sick.
Responding to patients is never a bother for us. AtlantiCare’s Emergency Medical Services and Heart and Vascular Institute teams provide care 24/7, 365 days a year. When it comes to surviving a heart attack, a key is in the door to balloon time. The American Heart Association’s standard time is 90 minutes. This time period is from when a patient arrives at the Emergency Department to when a cardiac catheterization team opens a blocked artery. AtlantiCare paramedics can begin the lifesaving treatment at the scene before arriving at the emergency department. Our time-saving care significantly contributes to AtlantiCare’s average door to balloon time is 56 minutes. That’s why dialing 911 is so critical.
Patients and family members need to understand and act on the symptoms they are experiencing. Symptoms aren’t always as dramatic as what you might have seen on television and in other media. Not everyone has crushing or stabbing chest pain, though some do. Some people have subtle symptoms. Chest pain or discomfort could go away in a few minutes or go away and come back. Some patients describe it as uncomfortable pressure or fullness. Feeling weak, light-headed, or faint; and breaking out into a cold sweat are symptoms. Pain or discomfort in the jaw, neck, or back can signal a heart attack. Shortness of breath is another sign.
You know your body better than anyone does – including when something just doesn’t feel right. For your heart’s sake, dial 911 for symptoms of heart attack.

